The Idea That Changed Cancer Treatment Forever
Four Keck Medicine of USC oncologists share how they’re working to make cancer a thing of the past through personalized medicine.
It was in Germany some 150 years ago that physicians started to categorize cancers based on where they originated: places like the breast, liver and bone. That system worked well enough for more than a century, guiding doctors in how they treated cancer and even prevent it.
But the approach has changed. “Maybe there’s a better way to do it,” says USC oncologist David Agus.
And it’s based on what switches cancer on or off—the drivers that help each tumor survive and thrive—not where the cancer lives.
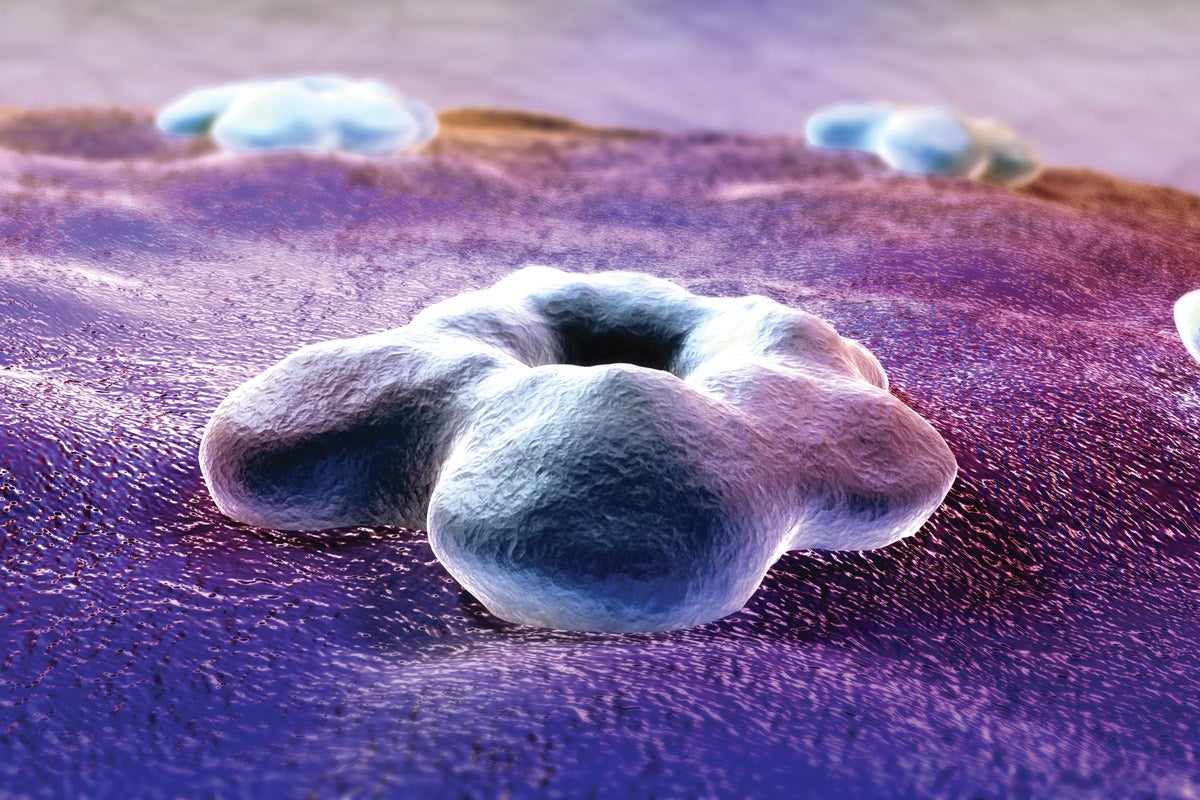
That’s the premise of personalized medicine, a cancer treatment strategy on the rise. The aim of personalized medicine is to get into each patient’s cancer at a molecular level. It asks, what’s going on with this cancer’s genes? Its proteins? Its chemistry?
The goal, Agus says, is to identify the genetic mutation that turned each patient’s cells cancerous, or a particular chemical process cells are “addicted to”—something the cancer needs to grow and spread. Then, doctors can pick a treatment precisely tuned to that mutant gene or key process. Sometimes personalized medicine aims to stoke a patient’s body to attack its cancer.
“It is a very exciting time with major developments in science that are rapidly impacting individuals with cancer,” says oncologist Alan Wayne of USC Norris Comprehensive Cancer Center and Children’s Hospital Los Angeles.
USC Trojan Family Magazine recently spoke with Wayne, Agus and two more of Keck Medicine of USC’s top cancer doctors about the promise of personalized medicine, and what’s coming up next.
CATEGORIZING CANCERS
HEINZ-JOSEF LENZ
Oncologist, Gastrointestinal Cancers
Until recently, everyone with colon cancer got the same treatment based on the cancer’s pathology alone, says oncologist Heinz-Josef Lenz. But recent advances in technology illuminate other characteristics of cancer beyond pathology, such as tumors’ molecular makeup. These new data influence how physicians prescribe therapy.
Lenz authored some of those very studies. Earlier this year, he shared his analysis of colon cancer types based on gene expression at the American Society of Clinical Oncology’s annual meeting, a major summit of top cancer experts. Looking at 800 genes across 392 tumors from patients, he and his colleagues found that these cancers fall into four genetically distinct groups. Each of these four cancer types acts completely differently and is driven by its own pathway, Lenz says. Each also has a distinctive prognosis and responds differently to chemotherapy and targeted drugs.
For example, people with cancer in one category tend to live longer if they receive a medication called cetuximab, which prevents the tumor from interacting with a growth factor, a substance in the body that helps the tumor get bigger. But people whose cancer falls into another category do better on a drug called bevacizumab, which interferes with the growth of blood vessels that fuel a tumor.
He has also found a difference between colon cancer types that he can’t explain with genes. Surprisingly, he says, “the location of the primary tumor is very important.”
Some tumors form on the right side of the colon, he explains. People with these right-side tumors do best on bevacizumab. Other tumors form on the left side, where the colon descends. Those patients have longer survival, Lenz found, and cetuximab helps them more.
“Even with DNA or RNA analysis, we cannot explain the significant difference between right- and left-sided colon cancers,” Lenz says. He’s now looking into other possible explanations to distinguish left- and right-side cancers. It might be related to something called methylation, he suspects. Cells attach chemical groups called methyls to genes to turn them on or off, and perhaps patterns of methylation will help explain the left-right difference. But only further research will tell.
CUSTOM CELL THERAPY
ALAN S. WAYNE
Pediatric Oncologist
Ask Wayne what he’s enthusiastic about, and he immediately talks about immunotherapy—a treatment that uses the immune system against cancer.
He’s working on a treatment that aims to super-charge each patient’s immune cells. It’s called CAR T-cell therapy.
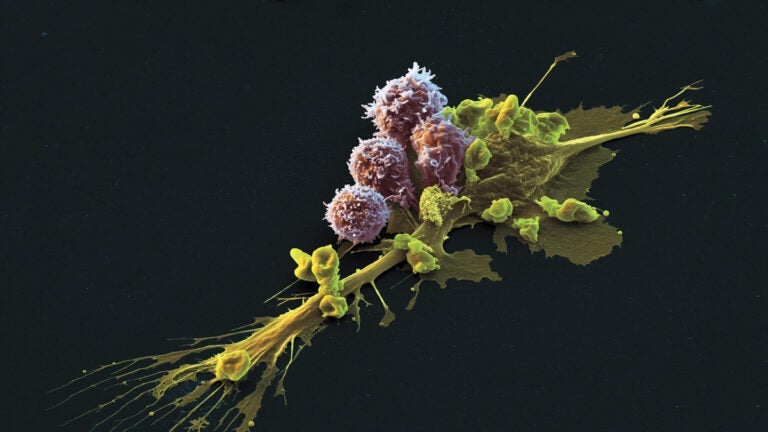
As part of the immune system, T cells circulating in the blood recognize and attack invaders. But cancer cells sometimes sneak by them. In CAR T-cell therapy, doctors take T cells from a patient’s bloodstream and send them for genetic engineering. Scientists add a new gene made of different parts, encoding a receptor that will identify the cancer as an enemy. The souped-up cells are transfused back into the patient, where they seek and destroy the cancer.
Wayne has been testing the approach in children with leukemia and other blood cancers. “It is a very exciting time,” he says, pointing to the August FDA approval of Kymriah, a CAR T-cell therapy. Children’s Hospital Los Angeles (CHLA) is one of a select group of sites now offering Kymriah, which was the first FDA-approved gene therapy available in the U.S.
While at the National Cancer Institute, Wayne led the development of one of the first trials of CAR T-cell therapy in children, with a different version than Kymriah, and he was encouraged by the results. Of 21 children and young adults who underwent the treatment, 14 achieved remission. Some of those kids had been expected to die, Wayne says; six had never responded to any other chemotherapy. He is now the lead principal investigator on a larger study to test this CAR T-cell treatment in children with leukemia.
Wayne and a team of investigators led by Jaclyn Biegel, professor of pathology at the Keck School and director of the Center for Personalized Medicine at CHLA, are employing gene sequencing technologies in a new way to identify genetic alterations in children’s cancers. Cancers in kids and teens often result from different mutations than tumors in adults, he explains, so his colleague Timothy Triche, professor of pathology at the Keck School, and a team of CHLA scientists worked with a company to develop a panel to detect the key gene abnormalities associated with children’s cancers. Their sequencing panel, called OncoKids, can identify cancer-related abnormalities in more than 500 genes. For children whose cancers do not respond to standard treatments, OncoKids can help doctors design a more personalized approach, choosing drugs that target the specific mutations found in that cancer.
IMPROVING IMMUNOTHERAPY
PREET CHAUDHARY
Hematologic Oncologist
In clinical trials, CAR T-cell therapy shows impressive results, often helping as many as 90 percent of patients and saving people who would likely otherwise die of their cancer. This is thanks to lots of logistical work, Preet Chaudhary points out. Scientists had to figure out how to gather the T cells from the patients, modify them and put them back in, all in a streamlined fashion that could be used for therapeutics. He predicts that in the future, this process will become more and more automated, making it easier for doctors to prescribe and provide CAR T-cell therapy.
But exciting as it is, CAR T-cell therapy comes with serious side effects and risks, Chaudhary says. It can cause the immune system to overreact, sometimes badly enough to result in death. It can be toxic to the brain, causing symptoms such as hallucinations, seizures and comas. And the genetically engineered cells only last for a few months to a year, so patients often relapse.
The reason, Chaudhary believes, is that the new receptors added to the cells are “Frankenstein” proteins, stitched together rather simply. “Like Frankenstein’s monster, they do work, but then they sometimes get out of control, and occasionally they can even kill you,” he says. But he also points out that in the short term, CAR T-cell therapy will remain an extremely promising treatment approach for a number of patients.
For the long term, he believes the solution will be found in the more elegant receptors that his lab group has designed, which he thinks will last longer and be less toxic. Early lab studies already show that Chaudhary’s engineered T cells can fight cancer. Now, he hopes to conduct further animal studies and start clinical trials in people, to test whether they work for longer periods with fewer side effects.
TARGETING CANCER EVERY WHICH WAY
DAVID AGUS
Medical Oncologist
Imagine you’re planning a trip from L.A. to San Francisco, Agus says. How long will it take you to get there? That depends on a lot of factors—your car’s gas mileage, the time of day you leave, the weather, roadwork and even your bladder capacity.
Understanding the tumor environment is just a sliver of what’s going on at the Ellison Institute and Keck Medicine.
At the Ellison Institute, which Agus and colleagues founded in 2016, researchers take the same approach to cancer. They want to know every factor that might contribute to how it grows, and how to stop it. And this isn’t just a job for biologists and doctors. The institute brings in physicists, mathematicians and engineers to inspire new approaches. Computers, crunching data ranging from genetic sequences to the organization of cells in a tumor, are a big part of the equation.
Agus is also excited about research that looks beyond the tumor to its immediate environment in the body. What helps it grow? What gets in its way?
As an example, Agus cites a clinical trial that studied women who had been treated for breast cancer. Breast cancer often moves into bone, so doctors gave half the women an osteoporosis medication to build up their bones. It turned out that the cancer was 40 percent less likely to return among the women who took the bone-building medicine. Something about strengthening the bone kept cancer cells from establishing themselves there.
“If you change the soil, the seed doesn’t grow,” Agus explains. Now, he adds, that osteoporosis drug is standard treatment for any cancer that tends to move into bone.
Understanding the tumor environment is just a sliver of what’s going on at the Ellison Institute and Keck Medicine. The doctors not only treat patients locally, but also work with physicians all over the world to promote personalized medicine techniques, Agus says. “We’re learning now how to treat and target the right tumor, with the right drug, at the right dose, in the right patient.”